
Repeated Postoperative Adhesive Small Bowel Obstruction Treated with Daeseunggi-tang and Acupuncture Treatment in Elderly: A Case Report
Ⓒ The Society of Pathology in Korean Medicine, The Physiological Society of Korean Medicine
Abstract
Postoperative adhesive small bowel obstruction (ASBO) is an intractable disorder which sometimes leads to adhesiolysis or small bowel resection. These therapeutic reoperations, however, also have many limitations including complications. An 80-year-old female, who had undergone 4-abdominal surgeries, visited the hospital with continuous vomiting. Based on her clinical symptoms and history, multiple air-fluid levels and distention of the small bowel in an abdominal X-ray, we diagnosed her with postoperative incomplete ASBO. We conducted acupuncture and an herbal medicine enema to stimulate bowel movement and relieve pain. The patient came in complaining of abdominal pain and vomited more than 10 times on hospital day 0 stopping on hospital day 4. Comparing hospital day 0 with hospital day 4, the abdominal pain decreased from a numerical rating scale (NRS) 10 to 4. There were no side effects such as redness or burns during the treatment process. This study presented an acupuncture-based treatment will be helpful for clinicians managing cases of ASBO with poor performance in elderly individuals.
Keywords:
Acupuncture, Herb medicine, Adhesive small bowel obstruction, Postoperative treatment, Case reportIntroduction
Intestinal obstruction is a phenomenon in which parts of the small intestine or large intestine are partially or completely blocked, thereby substances such as fluid or gas cannot flow out and thus accumulate.1) Many patients who undergo abdominal surgery experience intestinal adhesion with rates of approximately 63-97%.2) The symptoms of adhesive obstruction mainly include abdominal pain, nausea, vomiting, constipation, and/or abdominal distention and various factors, such as age, sex and comorbidity, affect the severity of symptoms.1) Some surgeons suggest timely reoperation because postoperative adhesive small bowel obstruction (ASBO) has poor prognosis peritonitis, strangulation and ischemia develop.3) However, approximately 90% of ASBO patients show improvement in symptoms with conventional management, nasogastric tubes, intravenous supplementation with fluids and electrolytes, and antispasmodic treatment.4)
Therefore, the World Society of Emergency Surgery ASBO working group recommends conservative treatment for ASBO in the first 72-h period, unless an emergency occurs.5) Nevertheless, some surgeons still argue that delayed surgery increases the recurrence of ASBO.6) From a geriatric perspective, reoperation carries many risks, such as psychological anxiety and depression, a high mortality rate and complications, a lower quality of life (QoL) and a long recovery period.7,8) In fact, both patients and caregivers generally choose nonoperative managements, especially in elderly ASBO patients. Accordingly, there are medicinal requirements of any effective nonoperative treatments or management for patients with ASBO.
Then, acupuncture therapy has been proposed as an effective option to reduce the complications after abdominal surgery.9,10) At this time, there is no manual for herbal medicine and acupuncture treatment for small intestine obstruction.
To communicate the potential of acupuncture-based management of ASBO, we herein report an elderly patient who recovered from severe symptoms of ASBO.
Case
1. Case presentation
This study was approved by the institutional review board (IRB) at Daejeon Korean Medicine Hospital (IRB number: DJDSKH-21-E-24)
An 80-year-old female Buddhist priest was admitted to a Korean Medicine Hospital because of abdominal pain, severe and persistent nausea/vomiting and abdominal distension. The patient had been overstrained due to preparation for the Buddha birthday festival. The patient suddenly experienced nausea and vomited several times a few hours later after eating spinach soup 2 days before visiting the hospital. The symptoms gradually worsened, and then the patient started to vomit a deep green liquid continuously with a small amount of finely chopped spinach at the time of visiting the hospital.
During an interview on her medical history, we noted that she had undergone 4 abdominal and pelvic surgeries (Fig. 1B). First, a subtotal gastrectomy was performed after a diagnosis of gastric cancer in her thirties, without any other cancer-related treatment. The patient also received a cholecystectomy for gallstones in her thirties. The patient was diagnosed with uterine cancer and underwent a hysterectomy at 54 years of age, with no other subsequent treatments related to the cancer. Next, at 69 years of age, the patient had a rupture of the bladder, received related pelvic surgery, and a Foley catheter was inserted. Additionally, she was in a traffic accident when she was 74 years old; the patient suffered multiple fractures of the ribs and right leg; and a compression fracture at the 2nd lumbar vertebra. After this accident, the patient had difficulty ambulating, making her dependent on wheelchairs for most of her daily life. The patient was diagnosed with hypertension, depression and insomnia at 77 years of age. At 79 years of age, a year before admission, the patient complained of the same symptoms that she currently presented, was diagnosed with ASBO at a Western-based hospital and received conservative treatment. The patient was taking medications for hypertension, incontinence, depression, insomnia and arthritis. The patient had a normal cognitive state and strong social and financial support.
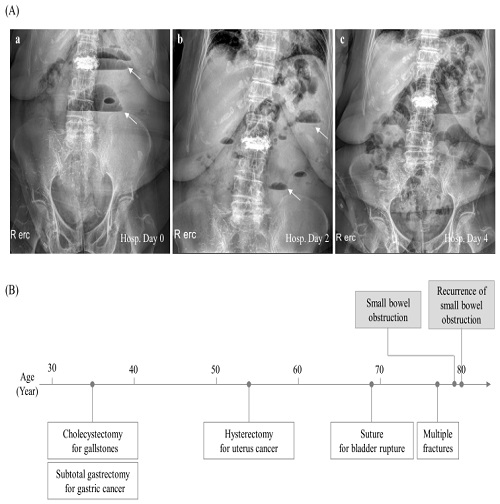
Summary of medical history and abdominal X-ray findings. (A) The sequential findings of abdominal erect X-ray are presented. Air-fluid levels are marked by white arrows. Hosp; Hospital. (B) The medical history was summarized.
When the patient visited the hospital, the patient presented a body temperature (36.9 ℃) in a normal but had hypertension (blood pressure 196/114 mmHg). The patient presented a distended abdomen, decreased bowel sounds, and pain with percussion, which was in accordance with findings from a simple abdominal X-ray showing multiple air-fluid levels, distention and gas collection in the small bowel loops, and only a little gas in the colon (Fig. 1A-a). The laboratory results were within the normal range for blood glucose levels, electrolytes, liver function tests and creatinine levels, except for a slight increase in blood urea nitrogen (BUN) levels (25.5 mg/dL) and C-reactive protein (CRP) levels (1.49 mg/dL), respectively. The erythrocyte sedimentation rate (ESR) was increased at 36 mm/hr, but the other parameters were within the normal range for the complete cell count (CBC) (Sup. Table 1).
2. Diagnosis
The authors diagnosed the patient with partial ASBO based on the typical radiography findings on the first abdominal X-ray and her symptoms. The patient was be able to be diagnosed with ABSO because their X-ray showed multiple air-fluid levels, distention and gas collection, which are the specific findings of small bowel obstruction, in the small bowel loops. The normal WBC count, electrolyte levels and body temperature and the small elevation of CRP did not indicate an emergency state that demanded immediate surgery, such as peritonitis, strangulation, or ischemia.
In addition, we ruled out acute appendicitis through the intensity and location of abdominal pain as complained about by the patient and the physical examination of the patient’s abdomin. In addition, acute gastritis and pancreatitis were excluded through examining the patient's usual eating habits and medications being taken. In Korean medicine, we identified the pattern as being cold-heat complex pattern. Not only could it be perceived as a deficiency-cold pattern in that the patient has undergone more than four intraperitoneal surgeries, old age and decreased appetite, but it can also be seen as an excess-heat pattern in that the symptoms have recently occurred and the measured blood pressure was high. Therefore, cold and heat were identified as being mixed without being biased to either side.
3. Treatments
We, members of the Korean Medicine Hospital as Korean medicine doctors, let blood at acupoints (SP1, LR1 and SI1) using lancets just after the patient arrived at our hospital. In addition, we performed manual acupuncture treatment based on meridian and acupoint theory two times per a day for four days using needles (diameter, 0.25 mm; length 30mm; Dongbang Healthcare Products, Seoul, Republic of Korea) at both sides of SiGuan (LI4, LR3) and ST36, ST40, SP3 at an approximate depth of 50mm for 20 minutes. Electric moxibustion (Ettum, TechnoScience, Seoul, Republic of Korea) was performed at CV8 (see Fig. 2A for acupoints). During hospitalization, the patient underwent daily acupuncture and moxibustion. The patient was given parenteral nutrition (5% dextrose saline) and an antispasmodic agent (tiropramide HCL 50 mg, im) with nothing per os (NPO) except for an angiotensin Ⅱ receptor antagonist to treat her high blood pressure. The patient had glycerin enemas; however, we did not insert a nasogastric tube due to the strong refusal of the patient.
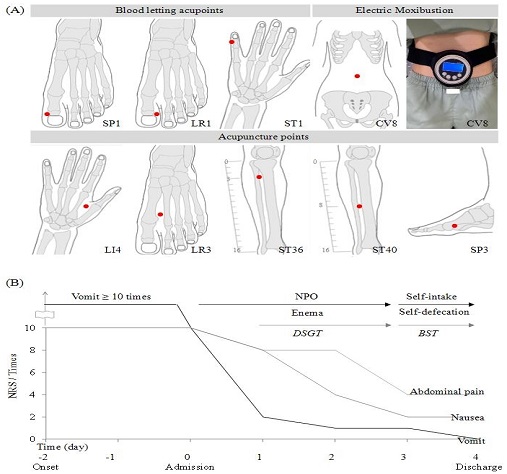
Summary of treatment and clinical outcomes. (A) Location of used acupoints. SP1; On the medial side of big toe, corner of the nail, LR1; On the lateral side of big toe, corner of the nail, ST1; On the medial side of 5th finger, corner of the nail, CV8; On the umbilicus, LI4; On the dorsum of the hand, between the 1st and 2nd metacarpal bones, LR3; On the dorsum of the foot, between the 1st and 2nd metatarsal bones, ST36; On the front side of the calf, 3/16 division from the knee joint to the ankle joint, ST40; On the front side of the calf, 8/16 division from the knee joint to the ankle joint, SP3; On the medial side of the foot, proximal fold of the 1st metatarsal bone. (B) DSGT; Daeseunggi-tang(Dachengqi-tang) BST; Banhasasim-tang(Banxiaxiexin-tang), NRS; numerical rating
4. Treatment responses
On hospital Day 0, the patient vomited 5 more times; and 2 more times at night. The patient initially said, "I keep vomiting and my mouth is dry. My stomach feels tight.". On hospital Day 1, we applied enema using Daeseunggi-tang (Dachengqi-tang)(DSGT)-mixed liquid to stimulate peristalsis, and the number of vomiting events and degree of nausea were remarkably decreased. On hospital Day 2, the symptoms improved, and we noticed a positive response on the abdominal X-ray(Fig. 1A-b). Then, the patient self-defecated during the night. On hospital Day 3, we stopped intravenous supplementation and started a soft diet with the prescription of Banhasasim-tang (Banxiaxiexin-tang) (BST). On hospital Day 4, we confirmed that the abdominal air-fluid level had almost disappeared and that there was some gas in the colon instead (Fig. 1A-c), and the patient was able to consume an oral diet and self-defecate. Later the patient said, "I didn't vomit more and my stomach feels less tense and more comfortable." During the treatment process, there were no side effects such as skin rashes, burns, infections, or additional digestive system symptoms. The patient was discharged slightly earlier than we recommended after a 4-night hospitalization(summarized in Fig. 2B).
NRS was used to check the degree of abdominal pain and nausea. The patient explained the degree of abdominal pain and nausea every day for four days. The abdominal pain was given a score of 10 on the NRS on hospital day 0, 8 on hospital day 2, and 4 on hospital day 4, indicating a decline. The other NRS, which showed the level of nausea, decreased from 10 on hospital day 0 to 4 on hospital day 2 and then to 2 on hospital day 4.
Discussion
We herein present a case of an elderly female patient who recovered from ASBO after acupuncture-based therapy without any complications. This case report provides clinicians with a cure and understanding of ASBO and the potential of acupuncture in elderly patients with ASBO.
Adhesive obstruction is defined as abnormal fibrous bands; between the intestine and tissue or both in the abdominal cavity that are separated in the normal state, resulting in mechanical obstruction.11) Adhesions mostly come from a pathological healing response of the peritoneum after abdominopelvic surgery.12) It is known that the occurrence risk of ASBO persists 10 to 20 years after surgery, and ASBO frequently recurs in up to 15.9% of patients.13,14) As observed in the present patient, it is estimated that up to 100% of patients who undergo abdominopelvic surgery experience mild ASBO.15) Furthermore, the recurrence risk of ASBO is known to be highest (34.6%) after gynecological surgery.2)
We may hypothesize that the recurrence of ASBO might have been caused by physical and psychological exhaustion when preparing for a religious holiday as well as her vegetarian diet, which is an inducer of ASBO.16) During the first diagnostic process, her previous cholecystectomy-related condition was ruled out by the normal range of total and direct bilirubin, ALP and γ-GTP along with other inflammatory parameters, such as ESR, WBCs and body temperature. The patient had chronic constipation and fecal impaction-related diseases, which are common in elderly individuals.17) However, a simple X-ray of the abdomen clarified the cause of her symptoms. The possibility of malignant tumor recurrence was also suspected; however, it was also ruled out by her laboratory findings.
We first conducted bloodletting acupuncture just after she arrived at our hospital at three acupoints (SP1, LR1 and SI1) for relieving severe abdominal pain and nausea. This therapy has been known to be effective for breaking energy stasis, cooling down energy, facilitating blood circulation, removing edema, supplying tissue oxygen, relieving pain, and recovering consciousness, depending on the acupoints.18) SP1, LR1 and SI1 are the first starting acupoints of the spleen, liver and small intestine meridians, respectively. Based on the conduit system for energy circulation of traditional Korean medicine, stimulating these acupoints rapidly activates the whole meridian energy, which is usually applied for severe and emergent diseases.19) Acupuncture at Siguan (both LI4 and LR3) modulated gastrointestinal motility in a randomized controlled clinical study.20) Acupuncture at ST36 and ST40 decreased inflammation-related cytokines (tumor necrosis factor-alpha and interleukin-6), which led to alleviation of inflammation-caused pain.21,22) SP3 is also known to enhance parasympathetic function.23) Besides, acupuncture treatment, we applied moxibustion at CV8, which has a beneficial effect on the recovery of gastrointestinal function.24)
In paralytic ileus or obstruction, enema administration could be an option helping the relief of the obstructive condition.25) We, therefore, applied an herbal decoction DSGT-mixed liquid for the enema, and it helped the passage of stool in the present case. DSGT is an herbal decoction, that has the therapeutical action of saline cathartic and anti-inflammation.26) In order to relieve the epigastric pain of the patient, we prescribed another herbal syrup BST. BST was well known to neutralize gastric acid and improves gastric smooth muscle movements.27-29) The composition and dose of DSGT and BST are presented in Table 2.
This 80-years aged patient was characterized as the 6th stage of the clinical frailty scale (living with moderate frailty), which classifies the elderly medical state into 9 stages (a higher stage represents a high risk of mortality.30) From a medical perspective, the patient further relied on polypharmacy and psychologically had a mood disorder. After comprehensive consideration, the patient needed conservative and effective treatment, and then she quickly recovered at our hospital. Fortunately, no adverse or unanticipated events occurred during hospitalization, and the patient responded well to acupuncture, moxibustion and herbal medication. The patient and her caregiver were satisfied with the especially acupuncture-based therapy. The patient has been still doing well with the normal daily activity, 4 months after discharge.
This case report reports one case. Continuous case reporting and research are required in the future. In particular, herbal medicine and acupuncture treatment are reported to have been effective for treating ABSO without any side effects, providing the possibility for future korean medical treatment.
References
-
Rami Reddy SR, Cappell MS. A Systematic Review of the Clinical Presentation, Diagnosis, and Treatment of Small Bowel Obstruction. Curr Gastroenterol Rep. 2017;19(6):28.
[https://doi.org/10.1007/s11894-017-0566-9]

-
Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999(9163);353:1476-80.
[https://doi.org/10.1016/S0140-6736(98)09337-4]

-
Teixeira PG, Karamanos E, Talving P, et al. Early operation is associated with a survival benefit for patients with adhesive bowel obstruction. Ann Surg. 2013;258(3):459-65.
[https://doi.org/10.1097/SLA.0b013e3182a1b100]

-
Schraufnagel D, Rajaee S, Millham FH. How many sunsets? Timing of surgery in adhesive small bowel obstruction: a study of the Nationwide Inpatient Sample. J Trauma Acute Care Surg. 2013;74(1):181-7.
[https://doi.org/10.1097/TA.0b013e31827891a1]

-
Ten Broek RPG, Krielen P, Di Saverio S, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;19(13):24.
[https://doi.org/10.1186/s13017-018-0185-2]

-
Foster NM, McGory ML, Zingmond DS, et al. Small bowel obstruction: a population-based appraisal. J Am Coll Surg. 2006;203(2):170-6.
[https://doi.org/10.1016/j.jamcollsurg.2006.04.020]

-
Jeppesen M, Tolstrup MB and Gögenur I. Chronic Pain, Quality of Life, and Functional Impairment After Surgery Due to Small Bowel Obstruction. World J Surg. 2016;40:2091-2097. 2016/07/08.
[https://doi.org/10.1007/s00268-016-3616-9]

-
Springer JE, Bailey JG, Davis PJ, et al. Management and outcomes of small bowel obstruction in older adult patients: a prospective cohort study. Can J Surg. 2014;57(6):379-84.
[https://doi.org/10.1503/cjs.029513]

-
Fu C, Wu T, Shu Q, et al. Acupuncture therapy on postoperative nausea and vomiting in abdominal operation: A Bayesian network meta analysis. Medicine (Baltimore). 2020;99(23):e20301. Available from: https://journals.lww.com/md-journal/Fulltext/2020/06050/Acupuncture_therapy_on_postoperative_nausea_and.14.aspx
[https://doi.org/10.1097/MD.0000000000020301]

-
Chen KB, Huang Y, Jin XL, et al. Electroacupuncture or transcutaneous electroacupuncture for postoperative ileus after abdominal surgery: A systematic review and meta-analysis. Int J Surg. 2019;70:93-101.
[https://doi.org/10.1016/j.ijsu.2019.08.034]

-
Ezzat RF, Rashid SA, Rashid AT, et al. Small intestinal obstruction due to phytobezoar: a case report. J Med Case Rep. 2009;3:9312.
[https://doi.org/10.1186/1752-1947-3-9312]

-
Duron JJ. Postoperative intraperitoneal adhesion pathophysiology. Colorectal Dis. 2007;9 Suppl 2:14-24.
[https://doi.org/10.1111/j.1463-1318.2007.01343.x]

-
Duron JJ, Silva NJ, du Montcel ST, et al. Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg. 2006;244(5):750-7.
[https://doi.org/10.1097/01.sla.0000225097.60142.68]

-
Fevang BT, Fevang J, Lie SA, et al. Long-term prognosis after operation for adhesive small bowel obstruction. Ann Surg. 2004;240(2):193-201.
[https://doi.org/10.1097/01.sla.0000132988.50122.de]

-
Chen SC, Lee CC, Yen ZS, et al. Specific oral medications decrease the need for surgery in adhesive partial small-bowel obstruction. Surg. 2006;139(3):312-6.
[https://doi.org/10.1016/j.surg.2005.08.020]

- Attard JA, MacLean AR. Adhesive small bowel obstruction: epidemiology, biology and prevention. Can J Surg. 2007;50(4):291-300.
-
Jung HW, Yoo HJ, Park SY, et al. The Korean version of the FRAIL scale: clinical feasibility and validity of assessing the frailty status of Korean elderly. Korean J Intern Med. 2016;31(3):594-600.
[https://doi.org/10.3904/kjim.2014.331]

-
Zhu QM, Yu NN, Liu BH, et al. Research advances in the clinical effect of bloodletting puncture at well-points in treatment of acute central nervous injury. Zhen Ci Yan Jiu. 2019;44(11):854-7.
[https://doi.org/10.13702/j.1000-0607.180167]

-
Yu NN, Xu ZF, Gao Y, et al. Wake-Promoting Effect of Bloodletting Puncture at Hand Twelve Jing-Well Points in Acute Stroke Patients: A Multi-center Randomized Controlled Trial. Chin J Integr Med. 2021;27:570-7.
[https://doi.org/10.1007/s11655-020-3093-8]

-
Shin KM, Park JE, Lee S, et al. Effect of siguan acupuncture on gastrointestinal motility: a randomized, sham-controlled, crossover trial. Evid Based Complement Alternat Med. 2013;2013:918392. Available from: https://www.hindawi.com/journals/ecam/2013/918392/
[https://doi.org/10.1155/2013/918392]

-
Oh JH, Bai SJ, Cho ZH, et al. Pain-relieving effects of acupuncture and electroacupuncture in an animal model of arthritic pain. Int J Neurosci. 2006;116(10):1139-56.
[https://doi.org/10.1080/00207450500513948]

- Le W, Xiao Y, Tian JY, et al. Effect of electroacupuncture at fenglong (ST40) on expressions of inflammatory factors in macrophages of hyperlipidemia model rats. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2013;33(10):1361-6.
-
Lee S, Chae Y, Kim SN, et al. Short term effects by acupuncture to SP3 on the autonomic blood flow control. Neurol Res. 2010;32 Suppl 1:37-42.
[https://doi.org/10.1179/016164109X12537002793887]

-
Yang L, Li Z, Li W, et al. Effects of moxibustion on gastrointestinal function recovery in preventing early postoperative small-bowel obstruction: a meta-analysis. Ann Palliat Med. 2021;10(4):3988-99.
[https://doi.org/10.21037/apm-20-1266]

-
Durai R and Ng PC. Catheter administered deep intestinal enema--case series. Acta Chir Belg. 2010;110(2):216-20.
[https://doi.org/10.1080/00015458.2010.11680602]

-
Ha KT, Kim JK, Lee YC, et al. Inhibitory effect of Daesungki-Tang on the invasiveness potential of hepatocellular carcinoma through inhibition of matrix metalloproteinase-2 and -9 activities. Toxicol Appl Pharmacol. 2004;200(1):1-6.
[https://doi.org/10.1016/j.taap.2004.03.012]

-
Kim SK, Joung JY, Ahn YC, et al. Beneficial Potential of Banha-Sasim-Tang for Stress-Sensitive Functional Dyspepsia via Modulation of Ghrelin: A Randomized Controlled Trial. Front Pharmacol. 2021;12:636752. Available from: https://www.frontiersin.org/articles/10.3389/fphar.2021.636752/full
[https://doi.org/10.3389/fphar.2021.636752]

-
Chen D, Zhao J, Cong W. Chinese Herbal Medicines Facilitate the Control of Chemotherapy-Induced Side Effects in Colorectal Cancer: Progress and Perspective. Front Pharmacol. 2018;9:1442. Available from: https://www.frontiersin.org/articles/10.3389/fphar.2018.01442/full
[https://doi.org/10.3389/fphar.2018.01442]

-
Yu Y, Zhang G, Han T, et al. Analysis of the pharmacological mechanism of Banxia Xiexin decoction in treating depression and ulcerative colitis based on a biological network module. BMC Complement Med Ther. 2020;20(1):199.
[https://doi.org/10.1186/s12906-020-02988-3]

- Byun YH, Park YS, Myung SJ, et al. Transient intestinal obstruction due to stool impaction in the elderly. Korean J Gastroenterol. 2005;46(3):11-7.
